Health
Health
In the past 75 years the human race has added 25 years to global life expectancy, significantly more than in the previous 10,000 years. These advances were realized through a monist atomist model of health and healthcare as we highlighted in our Living in a ⿻ World chapter. Such models (e.g. 'tropical medicine') were developed and refined through centuries of imperial and colonial governance, but their implementation worldwide was rapidly accelerated following the formation of the United Nations. This included achievements like the eradication of smallpox, the rapid expansion of immunizations including through Gavi the Vaccine Alliance, the massive expansion of antiretroviral therapy for HIV, and the recent reductions in maternal mortality through improvements in skilled birth attendance. Perhaps the most dramatic illustration of this model was that within two years of the appearance of COVID-19, 70% of world's population had received at least a single vaccine dose.
At the same time, progress in health-related Sustainable Development Goals (SDGs) has stalled or reversed[1], half the world's population lacks access to essential health services[2], impoverishing healthcare payments affect hundreds of millions each year[2:1], mental health services worldwide are severely underdeveloped[3], half of premature deaths are caused by non-communicable diseases[4] costing more than $2 trillion annually[5], and less than 3% of the world's population in some countries has access to basic assistive technologies (wheelchairs, walkers, canes, prosthetic limbs, eyeglasses, white canes, and hearing aids[6]. If we can address these social and intersubjective threats to health as effectively as we have the atomistic ones, we can easily add another 20 years to human life expectancy in the next century.
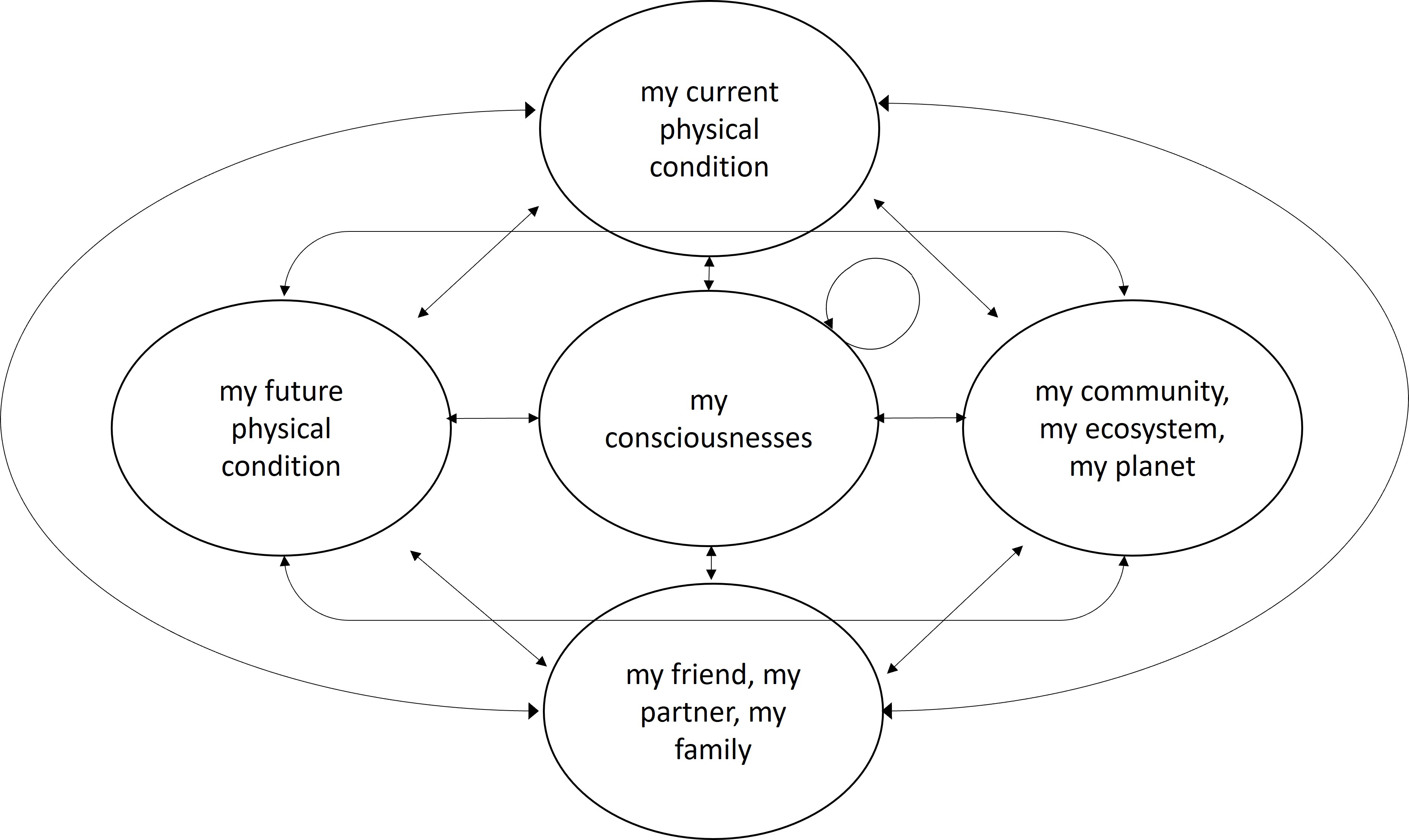
Achieving this goal, however, requires embracing a ⿻ concept of health (Figure A). Of course, the world will still need doctors, nurses, health facilities, laboratories, vaccines, drugs, and medical devices. But it also needs to empower the co-construction of health agency on the part of individuals and their communities, a term Jennifer Prah Ruger uses to describe the promotion of individuals' capabilities to act in their own interests with respect to their health[7]. However, health agency is rightly understood as primarily emergent, multiscale, embedded and complex (see our chapter Living in a ⿻ World ). In this view and as we now highlight, the central blockers to the next great era of human life extension are:
- Lack of financing
- Missing markets
- Coordination failures
- Missing communities
- Non-aligned incentives
- Lack of enabling services.
Reimagining health insurance
Health insurance allows people facing a range of risks to support their common health expenditures, both facilitating payments and evening out risk across time and people. While the role of insurance in "saving for a rainy day" is clear to most, the value of "pooling" risk across individuals is subtler: it facilitates both the collection of regular and predictable payments to offset unpredictable and sudden expenses and the redistribution from the better to the worse off.[8] This latter function of insurance is common to all expenditures intended to allieviate the suffering of the worse off, who from the "original position" prior to birth that John Rawls asks us to consider, are the victims of bad luck in their social or genetic position.[9]
Health insurance in practice varies along the three dimensions of prepayment, risk pooling, and redistribution. Private insurance in a competitive market faces the problem that insurers with better information can draw off lower-risk individuals by charging less, leaving the non-discriminating insurer with an 'adverse selection' of high-risk patients[10]. Private health insurance in a market economy thus tends to reduce to an actuarially informed health savings plan (i.e. with no risk pooling or redistribution), similar to self-managed Health Savings Accounts (HSAs) in the US.[11] This voids the HSA of most insurance value, including that of prudential savings, since individuals cannot calibrate their savings rates without actuarial information.
On the opposite extreme, "single-payer" national health insurance, financed from general government revenues and enacted through a compulsory and universal mandate, embodies the three elements of prepayment, risk pooling, and redistribution. However, such systems are rigidly based on a nation-state concept that is only one way of achieving pooling and redistribution at scale. For example, the Scandinavian countries admired for their socialization of risk have smaller populations than most large private health insurers in the US.
A natural alternative to this simplistic dichotomy of extremes precedes both in practice, namely social health insurance in which communities of solidarity care for those in need. Such a pattern is familiar to nearly everyone from their family lives, and it is not hard to understand how it extended to tribes and kin relationships. However, it also played a key role in classical Western civilization, such as the Roman collegia (the members of which co-deputize each other to act in their interests), where such family relations were extended to emerging urban social formations. Modern forms of social health insurance also emphasize the shared responsibility of a community for its members' healthcare costs and thus supplement individual, usually risk-adjusted prepayments, with collectivized contributions, usually not risk adjusted, from the employer (formerly, from the guilds, such as the medieval German knappschaften) and/or from another actor such as the state. Most health systems in the world predominantly follow either the social or the national insurance model, although private health insurance can be found virtually everywhere. Many current critiques of social health insurance object to i) financing healthcare from a tax on wages assessed through payroll deductions and ii) limiting entitlement to those who contribute such payments through the formal sector. Although there is merit in these concerns, it is useful to take a ⿻ perspective on social health insurance: there is a valid sense in which individuals who share a profession, or employer, and who therefore tend to share a common set of beliefs and values, should manifest a sense of solidarity that is particularly acute.[12]
Accordingly, we can reimagine health insurance as a '⿻ good' as in Social Markets: one that exhibits supermodularity in group size (especially across those facing diverse risks or life situations), but not requiring or even benefiting from universal participation. A ⿻ good builds on the strength of common belief across diverse scales and shapes embodied by ⿻ publics (see our chapter Association and ⿻ Publics). Of note is that the social model of health insurance began with the fact of 'association', namely, the creation of shared space for the enactment of common belief, shielded from full public surveillance and financed by ⿻ mechanisms. This reconceptualization allows for a dramatic expansion in the scope and role of insurance: rather than simply offering savings, risk smoothing or redistribution, ⿻ insurance might be used to finance the conditions required for health, rather than merely the payment of services to treat disease or infirmity. The more strongly a community interacts, the more likely it is to face common environmental or behavioral health risks, whether from the spread of communicable diseases, the ensuring of safe working conditions, the social spread of practices of healthy living or the creation of a healthy local natural environment. Health insurance might then look more like life insurance, and there is no strong reason for the two to be segmented and several strong reasons for them not to be.[13] Essentially, such an insurance fund could act as a mutual-aid society to foster coordination in the joint production of health rather than merely in its restoration: 'healthy minds in healthy bodies' but also healthy persons in healthy families and communities (see Figure A, above). Such a model, which we might call a "health production society", would ensure risk pooling and redistribution but could be much more relevant and effective at targeting the social determinants of health.
For example, it might be formed, in a developing country, to ensure the provision of clean water, sanitation, or adequate nutrition or in a wealthy country to mitigate the abuse of substances and ultra-processed foods that together account for 20 million global deaths a year.[14] The relevant needs are highly localized and, in fact, are often hard to address outside of a community context grounded in shared values, professional goals and belief systems. Or another such society might be formed on the global level for infections and globally transmissible diseases such as malaria, HIV or tuberculosis, such as the Global Fund to AIDS, Tuberculosis and Malaria. National reinsurers for local health production societies could help ensure that local networks most effective at interventions do not excessively fall prey to shared health risks. In short, a range of intersecting ⿻ health production societies could move beyond an atomistic, risk-based understanding of health to address the full range of social challenges in health, recognizing the pooling of risk as simply one example of supermodularity. Such societies would rely on the full host of technologies we have described above for building community consensus, common understanding/purpose and shielding action from outside surveillance (such as by a national insurer) that could undermine it.
Health impact tokenization
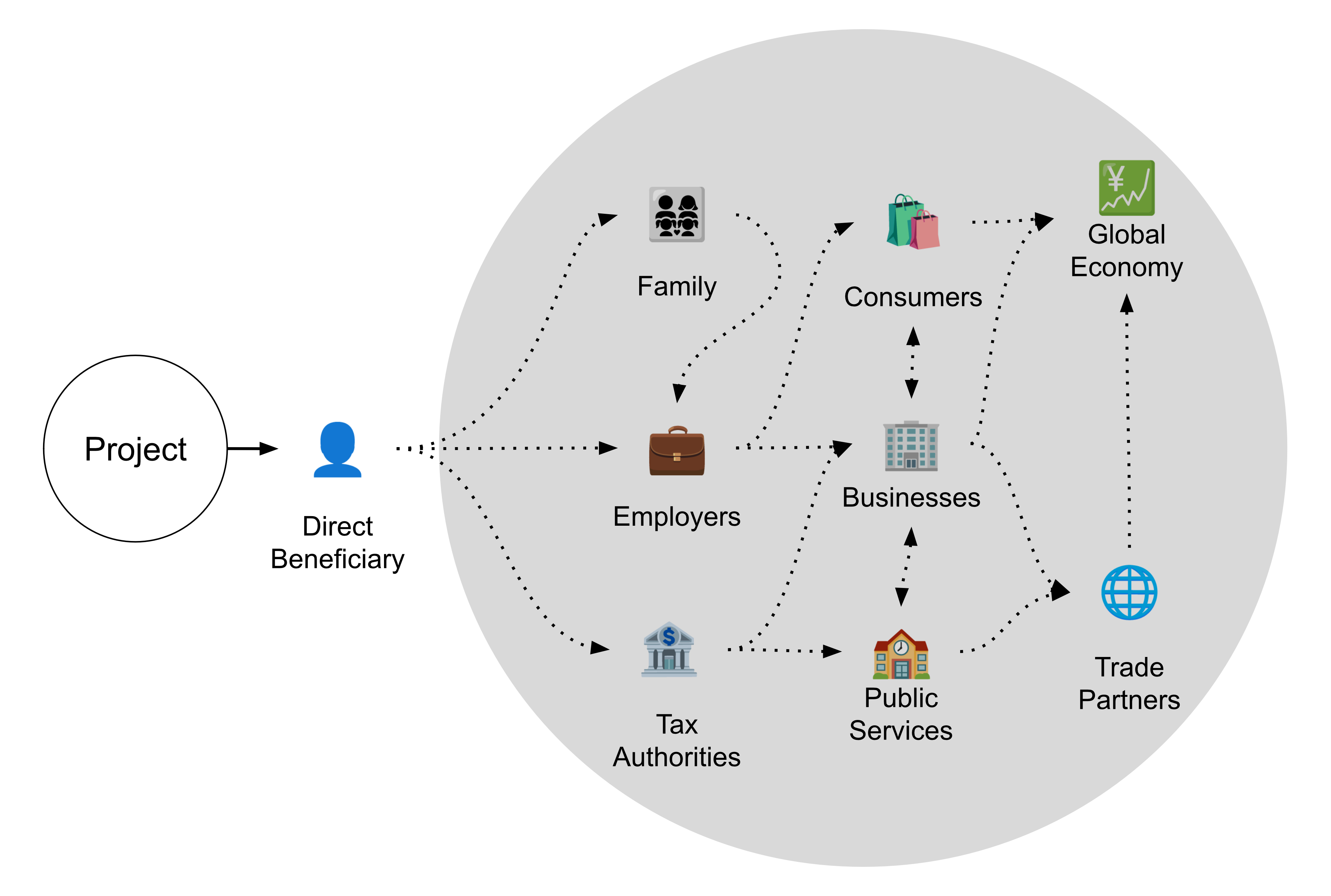
For the purpose of this discussion, outputs are the direct result of health services (e.g. people vaccinated); outcomes are the final intended result (e.g. deaths avoided through morbidity or mortality risk reduction); and impacts are the knock-on effects outcomes have in the world at large (e.g. future children born). Impact is thus an open-source commodity: it can be forked to whatever use the beneficiary can devise (Figure B). Although impacts are a causal effect of health services (e.g. a child who otherwise would have died did not, and then went on to be a parent), impacts are not the primary intended effect of health services. The primary intended effect of health services is reducing morbidity or mortality risk, which as we have seen is an insurance function. Health services, which produce non-market-traded outcomes (e.g. lives saved and healthier lives, through the insurance function) and market-traded and non-market-traded impacts (e.g. more labour to sell and more time for visits with friends, through the open-source function), thus have an accounting problem: it is hard to measure the value of outcomes (e.g. the value of a life saved) but it is often still harder to measure the value of relevant impacts. Thus, since the full social value of health projects is in practice never counted, let alone captured or rendered tradeable, many win-win health investments remain blocked.
For example, the Global Fund claims to have saved 44 million lives over 20 years at a cumulative cost of $55.4 billion in disbursements plus approximately $6 billion in operating costs funded primarily by governments and philanthropists. Median estimates for the insurance value of a mortality risk reduction of this scale would come in at about $200 trillion dollars, attributing to the Global Fund an (undiscounted) outcomes-based return on investment (ROI) of over 3000:1. Accordingly, if the Global Fund could have captured a fraction of the insurance value of the outcomes it produced, it would be one of the most valuable entities in the world today, and everyone would want to buy its shares. In fact, everyone in the world already does own non-tradeable shares in the Global Fund, which pays out regular dividends in the form of reduced rates of disease contraction, increased economic growth and the benefits of loved ones living fuller lives among many other things. The question is how to raise revenue against these implicit, untraded shares to fund investment that can increase the benefits they pay out.[15]
- We must be able to represent both the insurance and the broader social value of these investments. These can be tokenized based on digital certificates that use a combination of technocratic outcome evaluation, but also using "crowd-sourced" intelligence as highlighted, for example, in our ⿻ Voting chapter.
- Build on this to coordinate fragmented funders and implementers through open impact pools that address the shortcomings noted with existing health financing. Develop an open coordination standard for subscription to pools that addresses the drawbacks of current health financing. Tokens can be used to participate in the governance of projects or of the funding pools. Projects can allocate tokens linked to contributions. Tokens can be used to participate in governance; to trade and invest; to exchange for selected services; or to fund further projects.
- Harness generative foundation models (GFMs) and other applications to accelerate the process of forming such instruments and adapting them to particular investments. Through tokenization, bundling and trading, it can be made as simple to buy health impact as carbon credits. Tokens can be reinvested into projects or used to purchase health services according to a standardized impact model. Value can be linked to specific projects or aggregated into blocks, supporting the development of cascading ('fractal') health-impact markets.
Incenting equitable benefit sharing
Health insurance consists of pooled mechanisms for the prepayment for health services that reduce mortality or morbidity risk, with a flexible element of benefit and risk redistribution. Benefit sharing in particular has bedeviled blended-finance agreements that promised to mobilize additional sources of funds from private, profit-seeking actors; instead of mobilizing new sources of funding, however, existing arrangements have tended to allow private investors to capture the benefits of public de-risking while offering little or no financial incentive to ensure the active engagement of direct (or indirect) beneficiaries or to reward the commitment of, for example, biological, behavioural, or other services by stakeholders and participants. Open impact pools that allow for broad participation in governance including by beneficiaries themselves, and therefore also a broader entitlement to benefits through productizing benefit classes based on a standardized impact model, can more equitably distribute both risk and benefit and help incentivize the at-scale production of key ⿻ goods.
Deliberative tools for health cooperation
The world has experienced an increasing wave of pandemics, with 6 occurring already this century. In circumstances such as those in which COVID-19 emerged, one principle stands out: public health policy must be formulated in the presence of massive uncertainty about basic facts. For example, in early 2020, we knew we were confronted with two important unknowns: Q1. How long would it take to develop an effective COVID vaccine? and Q2. Would populations tolerate the imposition of social distancing measures? Policy-makers got these questions badly wrong, estimating "at least 18 months" for the first and "no" for the second when "5 months" and "yes" were closer to correct. In fact, diverse publics worldwide largely led government response rather than following it during February and March of 2020.
If diffuse populations of individuals or loosely organized non-health associations, such as soccer clubs, can formulate objectively better pandemic policy than a government that is advised by the world's top epidemiological experts, then governments are turning a blind eye to a critical source of information and analysis. The use of online tools such as expert-elicitation databases maintained on a variety of collaborative, deliberative, voting or prediction-market (i.e. 'governance') technologies as we described in our chapter on Augmented Deliberation would have multiplied by orders of magnitude the power of 'the wisdom of the crowd'.[16] Indeed, in the long run, more important than 'getting policy right' is preserving social cohesion and public trust in policy-makers since without these 'policy' rapidly becomes meaningless anyway. Taiwan followed a very different path, with rapid government support of citizen-led initiatives for, for example, tracking the supply of masks. By moving quickly to empower citizen-led online initiatives (g0v, Polis), Taiwan was able to harvest the power of localized and contextual knowledge as a ⿻ good without imposing centralized control while respecting privacy. Taiwan's "extitutional" approach was so successful that it has now been institutionalized. With eloquent examples such as these, it follows that policy-making during the next novel pandemic will not be the sole prerogative of epidemiological experts in closed-room consultations, and that ⿻ technologies will be widely used for the large-scale formulation of and coordination around collective action.
In virtually every part of the world, healthcare is administered through a model originating in colonizing powers, usually as a mirror of the forms of administration found in the respective imperial centers but with the additional mission of 'development' tacked on. Results have naturally been mixed. Nevertheless, in a number of former colonies, notably in Canada and Australia, concerted efforts are being made on the part of colonialist successor administrations to learn from Indigeneous models of health and healthcare, to engage in the co-administration of healthcare and other health services in accordance with Indigeneous community values, and to allow for the self-determination of solutions by Indigeneous peoples. As these experiments remain few and far between, GFMs seem a promising tool to leverage the large and diffuse bodies of textual data produced in these initiatives for the purpose of interpreting, criticizing, reimagining, and eventually redesigning, systems of healthcare administration to be more responsive to cultural value systems. As discussed in our chapter on Augmented Deliberation, "points of view" that are held (albeit diffusely) by organizations and even entire cultures can be represented as an "individual" whose "synthetic wisdom" can be queried in real-time interactions, or who can be tasked with designing incentive-compatible healthcare and interventions along a non-colonialist model.
Post-symbolic communication for health
Brain computer interfaces (BCIs, see our chapter Post-Symbolic Communication) are not some futuristic fantasy of science fiction but familiar objects in common use. The usual operating system is that of the sensory and motor organs. Eyeglasses and hearing aids are low bit-rate computing devices that interface (unidirectionally, or write only) with our brains through the sensory organs; canes, crutches and wheelchairs are low bit-rate mechanical computers that interface with the brain bidirectionally (i.e. read/write), through the intermediary of both the sensory and motor organs. Digital assistive devices, such as smart-phones or portable computers, are (slightly) higher bit-rate devices that interface with the brain (read/write) through the intermediary of the sensory-motor system (usually the visual, hearing and fine-motor systems) but also through higher-order domains of functioning such as speech (e.g. voice recognition), cognition (e.g. CAPTCHAs) and memory (e.g. passwords). These 'BCIs' interact through a range of input/output devices including keyboards, (touch)screens and a variety of other read/write interfaces. Such higher bit-rate digital computing tools have become for many people an indispensable part of what it means 'to be human': as anyone who has lost their smartphone knows, the experience is one of significant disability.
It would be futile to insist that such devices are not now an integral part of our (transhuman) personality.[17] Common applications of such technologies exist in the form of mobile health (e.g. text-message alerts, wearable devices, contact-tracing tools), telemedicine and telehealth (e.g. virtual fracture clinics)[18], and e-health (e.g. digital health records). It is natural and obvious that the trend towards further modalities of interactivity, and higher bit-rate throughput, will have in time important implications for health, especially for visual, hearing, mobility, self-care, and speech disorders, notably through Extended Reality (XR) services. Biomedical engineering is already working to connect prosthetic devices at cellular level (i.e. bionics)[19], and BCIs hold out the corollary promise of allowing for such connectivity at cognitive, emotional and experiential level with, for example, powerful applications in speech and communication disorders, in the enhancement (or maintenance) of cognitive functions such as memory and, almost certainly, in novel applications for common mental disorders such as depression and anxiety, as well as for impulse control for addictive disorders.
Immersive shared reality (ISR) has thus far primarily been used in non-interpersonal medical settings, such as to de-risk medical training for health workers, much as flight simulators do for pilots. It is natural, however, to imagine the gamification of health-based ISR so as to incent the learning of complex cognitive, relational, and behavioural skills (such as self-care, self-insight, and self-management), as well as a suite of simulated interpersonal applications (see our Immersive Shared Reality chapter). Similar to the examples cited there, new horizons of simulated and non-simulated social interaction can be opened to those with disabilities that less immersive, lower-throughput, traditional assistive technologies cannot address.
GFMs and data sharing to assist diagnosis and treatment
A human radiographer can at the upwards limit view and interpret perhaps as many one million diagnostic imaging scans during a lifetime of practice. While this is sufficient to achieve expert status in diagnosing common conditions, GFMs can fine-tune on datasets orders of magnitude larger and thus outperform human readers for the diagnosis of rarely seen conditions. Of course, human beings might specialize in such conditions and dedicate themselves to viewing a collection of many rare images, but the need for ⿻ technologies then becomes more acute: it seems impossible to imagine how large diagnostic databases of rare conditions can be compiled without established data-sharing practices across many image centres. In this case too, we see diffuse pockets of diversity that show 'affinity' in terms of markers that cannot be organized into low-entropy pockets based merely on traditional variables such as place, profession, or parentage; in these cases, another organizing principle must be found, and online technologies are the obvious solution. Such technologies also need to respect privacy and confidentiality, both as a normative and legal principle. Various forms of privacy enhancing technologies (see our chapter Association and ⿻ Publics) such as zero- (or low-) knowledge proofs, allow for specific kinds of information to be reliably shared without over-sharing, helping enable simultaneous respect for medical privacy and large-scale data sharing.[20]
In Web2 applications such as Facebook and Google, users "willingly" share their private information in exchange for the social benefits afforded by the platforms. That is, even knowing that their information is being harvested for profit by third-party entities, many individuals presumably still find that membership in online Web2 communities offers a net benefit. What if there was no trade-off between privacy and utility? What if accessing medical services did not incur an open-ended contingent liability for the privacy of the individual? Medical administrative data is 'safe' for everyone, until the system is hacked because of, for example, a phishing attack: in the long run, we all face data theft with Web2 systems. Rethinking medical practice (which requires patient data for the patient's own benefit) and medical research (which requires patient data for the benefit of others) so as to build in cryptographic principles from the foundation is an essential part of the Web3 project, with important health implications: no doubt some diseases today are still fatal only because of our failure to build such applications. Extending the diagnostic example, medical notes of all kinds (e.g. admission, treatment, discharge) forming a part of a patient's record are a potentially vast source of information about care and outcomes that is not only highly diffuse and unstructured but also virtually unqueryable outside of a set of specific and restricted medicolegal contexts. If there is a way to extract weak, or highly confounded, signals as the basis for novel causal insights, GFMs are perhaps the only technology that might do so. Variations in medical practice and outcomes should in principle make it possible to identify and extract the relevant counterfactual, much as - at population level - regression discontinuity design does. Such practices could transform a variety of medical practices, such as making post-approval regulatory changes far more dynamic and adaptive.
Given the enormous amount of value currently 'left on the table' by the under-production of health, it is critical that ⿻ technologies increasingly be used to:
- Unlock successive layers of value for health funders, implementers, and beneficiaries.
- Attract a broader group of health funders, implementers, and beneficiaries who will want to work with novel mechanisms to coordinate around funding and production of health goods.
- Empower the construction of health-oriented communities of practice by funders, implementers and beneficiaries.
- Ensure the reciprocal, symmetric, and equitable governance of pooled, co-created health assets by funders, implementers and beneficiaries.
- Enable new forms of international, regional and local cooperation in the co-production of health.
- Unlock new avenues for healthy human (and transhuman) functioning.
The blockers noted above (lack of financing, missing markets, coordination failures, missing communities, misaligned incentives, and lack of enabling services) will be overcome, and the dark clouds blocking the path to another 20 years of healthy life expectancy will dissipate the world over.
“The Sustainable Development Goals Report: Special Edition,” (New York: UN DESA, July 2023), https://desapublications.un.org/file/1169/download. ↩︎
“Tracking Universal Health Coverage: 2023 Global Monitoring Report,” (Geneva: World Health Organization, September 18, 2023), https://iris.who.int/bitstream/handle/10665/374059/9789240080379-eng.pdf?sequence=1. ↩︎ ↩︎
“Transforming Mental Health for All,” (Geneva: World Health Organisation, 2022), https://iris.who.int/bitstream/handle/10665/356119/9789240049338-eng.pdf?sequence=1. ↩︎
“Noncommunicable Diseases,” World Health Organization, September 16, 2023, https://www.who.int/news-room/fact-sheets/detail/noncommunicable-diseases. ↩︎
“Financing NCDs,” NCD Alliance, March 2, 2015, https://ncdalliance.org/why-ncds/financing-ncds. ↩︎
“Assistive Technology.” World Health Organization: WHO, May 15, 2023. https://www.who.int/news-room/fact-sheets/detail/assistive-technology. ↩︎
Jennifer Ruger, Health and Social Justice, (New York: Oxford University Press, 2010), pp. 276. ↩︎
In his 1991 Lindley Lecture, the philosopher Derek Parfit distinguished a novel theory of ethics, in contrast to either utilitarianism or egalitarianism, which he called "the priority view". Its main tenet is that the worse off have a special claim on resources. Prioritarianism (before the term) has been used by economists in the analysis of social welfare functions ('optimal taxation') since at least the 1970s. Prioritarianism is not usually considered - as it is here - as a form of insurance. ↩︎
John Rawls, A Theory of Justice, Revised edition, (Cambridge, MA: Harvard University Press, 1999). ↩︎
Kenneth Arrow, "Uncertainty and the welfare economics of medical care," American Economic Review 53, 5 (1963): 941-973. ↩︎
See Healthcare.gov, “Health Savings Account (HSA),” HealthCare.gov, 2019, https://www.healthcare.gov/glossary/health-savings-account-HSA/. ↩︎
Émile Durkheim, De la Division du Travail Social (Paris: Presses Universitaires de France, 1893). ↩︎
Robin Hanson, Buy Health, Not Health Care, Cato Journal 14, 1 (1994):135-141, Summer. ↩︎
Anna Gilmore, Alice Fabbri, Fran Baum, Adam Bertscher, Krista Bondy, Ha-Joon Chang, Sandro Demaio, et al., “Defining and Conceptualising the Commercial Determinants of Health,” The Lancet 401, no. 10383 (April 8, 2023): 1194–1213. https://doi.org/10.1016/S0140-6736(23)00013-2. ↩︎
In 2023, two of the contributors to this chapter created a Swiss-registered Association with the name Unexia that is pursuing the measures described here with a range of UN and other partner organizations. ↩︎
Kristin Shrader-Frechette, “Experts in Uncertainty: Opinion and Subjective Probability in Science.Roger M. Cooke,” Ethics 103, no. 3 (April 1993): 599–601, https://doi.org/10.1086/293541. ↩︎
Donna Haraway, "A Cyborg Manifesto: Science, Technology, and Socialist-Feminism in the Late Twentieth Century," in Simians, Cyborgs and Women: The Reinvention of Nature (New York; Routledge, 1991), pp. 149-181. ↩︎
Gillian Anderson, Paul Jenkins, David McDonald, Robert Van Der Meer, Alec Morton, Margaret Nugent, and Lech A Rymaszewski, “Cost Comparison of Orthopaedic Fracture Pathways Using Discrete Event Simulation in a Glasgow Hospital,” BMJ Open 7, no. 9 (September 2017): e014509, https://doi.org/10.1136/bmjopen-2016-014509. ↩︎
Laurent Frossard, Silvia Conforto, and Oskar Aszmann, “Editorial: Bionics Limb Prostheses: Advances in Clinical and Prosthetic Care Editorial on the Research Topic Bionic Limb Prostheses: Advances in Clinical and Prosthetic Care Context Importance of Residuum Health,” Frontiers in Rehabilitation Sciences 3 (August 18, 2022). https://doi.org/10.3389/fresc.2022.950481. ↩︎
Nicola Rieke et al. "The Future of Digital Health with Federated Learning" npj Digital Medicine 3 (2020): article 119. ↩︎